The anal canal is lined with small glands that normally secrete mucus to aid in bowel movements. When these glands become blocked or infected, an abscess can form. As the body attempts to drain this abscess, it may create a tunnel or tract from the infected gland to the skin surface, resulting in a fistula. If you’re experiencing symptoms of an anal fistula or other anorectal issues, it’s crucial to consult a Gastroenterologist in Chennai or your local area for proper diagnosis and treatment.
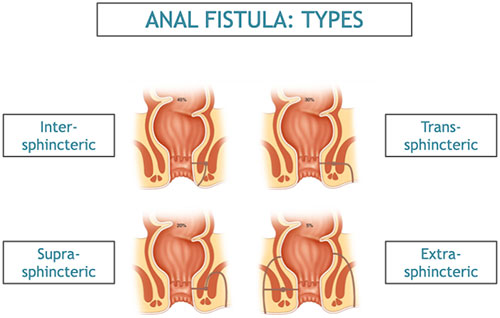
Types of Anal Fistulas:
Fistulas are classified based on their relationship to the anal sphincter muscles:
- Intersphincteric: Passes through the internal sphincter
- Transsphincteric: Crosses both internal and external sphincters
- Suprasphincteric: Tracks above and across the sphincter complex
- Extrasphincteric: Bypasses both sphincters entirely
Symptoms of Anal Fistulas:
- Persistent pain and swelling around the anus
- Continuous or intermittent drainage of pus or blood from the anal area
- Irritation and itching of surrounding skin
- Difficulty sitting comfortably
- Pain during bowel movements
- Fever and fatigue in cases of active infection
- Recurrent abscesses in the same area
Causes of Anal Fistula:
While a previous anorectal abscess is the most common cause, other potential factors include:
- Crohn’s disease and other inflammatory bowel conditions
- Tuberculosis
- Sexually transmitted infections, particularly HIV
- Trauma or surgery in the anal area
- Radiation therapy to the pelvic region
- Malignancies in rare cases
Risk Factors:
- Smoking
- Obesity
- Sedentary lifestyle
- Poor anal hygiene
- Chronic diarrhea or constipation
Diagnosis of Anal Fistula:
Accurate diagnosis is crucial for effective treatment. Methods include:
- Physical examination, including digital rectal exam
- Anoscopy or proctoscopy
- Fistulography: Injecting contrast material into the external opening
- Endoanal ultrasound: High-resolution imaging of the anal canal
- Magnetic resonance imaging (MRI): Detailed imaging of soft tissues
- Computed tomography (CT) scan: In cases of complex or recurrent fistulas
Treatment Options:
Treatment typically involves surgery to eliminate the fistula while preserving anal sphincter function. The choice of procedure depends on the fistula’s location and complexity:
- Fistulotomy:
- Opening the entire fistula tract
- Most suitable for simple, low fistulas
- High success rate but may impact continence for higher fistulas
- Seton placement:
- Inserting a thread-like material through the fistula
- Allows gradual healing and can be used as a staged approach
- Useful for complex fistulas or in patients with high risk of incontinence
- Advancement flap procedure:
- Creating a flap of tissue to close the internal fistula opening
- Preserves sphincter function
- Suitable for higher or more complex fistulas
- LIFT procedure (Ligation of Intersphincteric Fistula Tract):
- Accessing the fistula through the space between sphincters
- Relatively new technique with promising results
- Preserves sphincter function
- Fibrin glue and collagen plugs:
- Less invasive options
- Involve filling the fistula tract with healing-promoting materials
- Variable success rates, often used in combination with other treatments
- Stem cell therapy:
- Emerging treatment using autologous adipose-derived stem cells
- Shows promise in healing complex fistulas, particularly in Crohn’s disease
Postoperative Care and Recovery:
- Proper wound care is essential to prevent infection and promote healing
- Sitz baths can help soothe the area and maintain cleanliness
- Pain management may involve both oral medications and topical treatments
- Stool softeners are often prescribed to ease bowel movements
- Follow-up appointments are crucial to monitor healing and detect recurrence
Complications and Prognosis:
Potential complications include:
- Recurrence of the fistula
- Incontinence, particularly after complex surgeries
- Chronic pain or discomfort
- Scarring and anal stricture
Prognosis varies depending on the fistula’s complexity and chosen treatment. Simple fistulas treated with fistulotomy have high success rates, while complex fistulas may require multiple interventions.
Prevention and Lifestyle Considerations:
- Prompt treatment of anal abscesses to prevent fistula formation
- Management of underlying conditions like Crohn’s disease
- Maintaining good anal hygiene
- Avoiding excessive straining during bowel movements
- Balanced diet rich in fiber to promote regular bowel habits
- Regular exercise to improve overall health and circulation
Research and Future Directions:
Ongoing research focuses on:
- Improving surgical techniques to minimize recurrence and preserve function
- Developing new biomaterials for fistula closure
- Exploring regenerative medicine approaches, including stem cell therapies
- Investigating the role of the microbiome in fistula development and healing
Conclusion:
Anal fistulas represent a complex anorectal condition that requires a multidisciplinary approach for optimal management. While they can be challenging to treat, advances in surgical techniques and emerging therapies continue to improve outcomes for patients. Early diagnosis, appropriate treatment selection, and comprehensive follow-up care are key to managing this condition effectively and improving quality of life for those affected.